Assume you have two balloons filled with gas. You tie a thread to one balloon and hold it down while the other is free to float up into the sky.
Which one do you think will rise higher?
Obviously, the second one!
The same thing can happen with your teeth. While most teeth are free to move and erupt as they grow, sometimes a tooth gets trapped in the jawbone, unable to rise or move as it should.
This condition is called an ankylosed tooth in medical terms.
Ankylosed teeth are more commonly found in children and adolescents. They typically affect primary (baby) teeth, most often the lower molars, and are usually discovered when the baby tooth fails to fall out on its own or disrupts the permanent teeth’ eruption.
This condition can also occur in permanent teeth but is far less common. It often becomes noticeable during periods of tooth eruption (around ages 6 to 12), when the expected movement or shedding of baby teeth doesn’t happen normally.
In adults, ankylosis is rarer but can happen due to trauma, infection, or underlying bone conditions.
Why is an ankylosed tooth a big deal? Well, while it might seem like a small issue at first—after all, it’s just one tooth, right?—the reality is that an ankylosed tooth can cause long-term problems, especially if it’s left untreated.
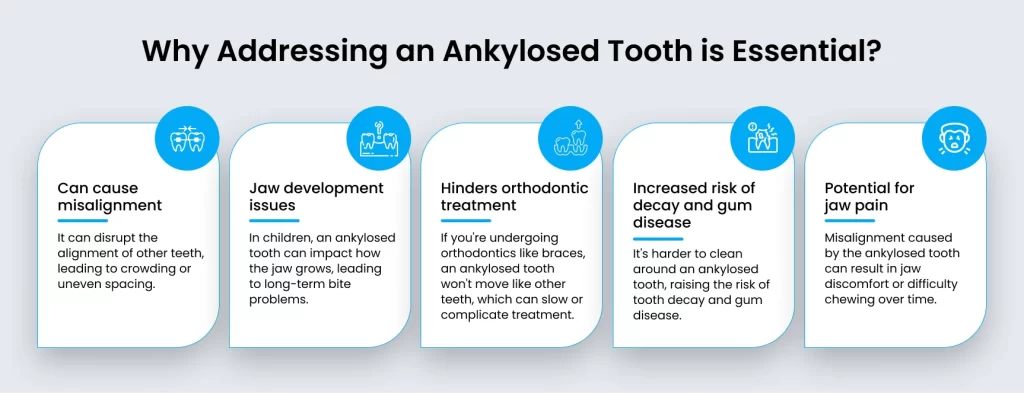
For starters, if the tooth is stuck in the jawbone, it doesn’t just affect that one tooth. Over time, it can disrupt the alignment of other teeth, cause crowding, or even impact how your jaw develops, particularly in children. This can lead to more serious issues like an uneven bite or jaw pain, making it harder to chew properly.
And here’s the thing—because the tooth is fused to the bone, it won’t move like the rest of your teeth. So if you or your child is going through orthodontic treatment, like getting braces, the ankylosed tooth could slow down progress or make it difficult to achieve the perfect smile you’re aiming for. In the long run, this can mean more time, effort, and potentially costly treatments down the road.
Leaving it untreated might also increase the risk of gum disease or tooth decay around the affected area, as it’s often harder to clean around an ankylosed tooth properly.
So, it’s definitely not something to ignore. The sooner it’s addressed, the better the chances of avoiding those long-term complications. If you notice any signs or feel like something’s off, it’s worth talking to your dentist about what’s happening. They’ll help guide you to the right treatment and ensure everything stays on track!
Sometimes, spotting an ankylosed tooth isn’t easy, especially because it doesn’t always cause obvious pain or discomfort at first. Many people may not even realize they have it until a dental exam. But there are a few signs you can look out for that may indicate something’s not quite right.

If you use Google to understand medical conditions, you might confuse an ankylosed tooth with an impacted tooth. Both are totally different. Here’s how.
Ankylosed Tooth vs. Impacted Tooth: What’s the Difference?
It’s easy to confuse an ankylosed tooth with an impacted tooth, but there’s a key difference.
An ankylosed tooth can cause different problems depending on whether it occurs in a child or an adult, and it’s important to understand how these age groups face unique challenges.
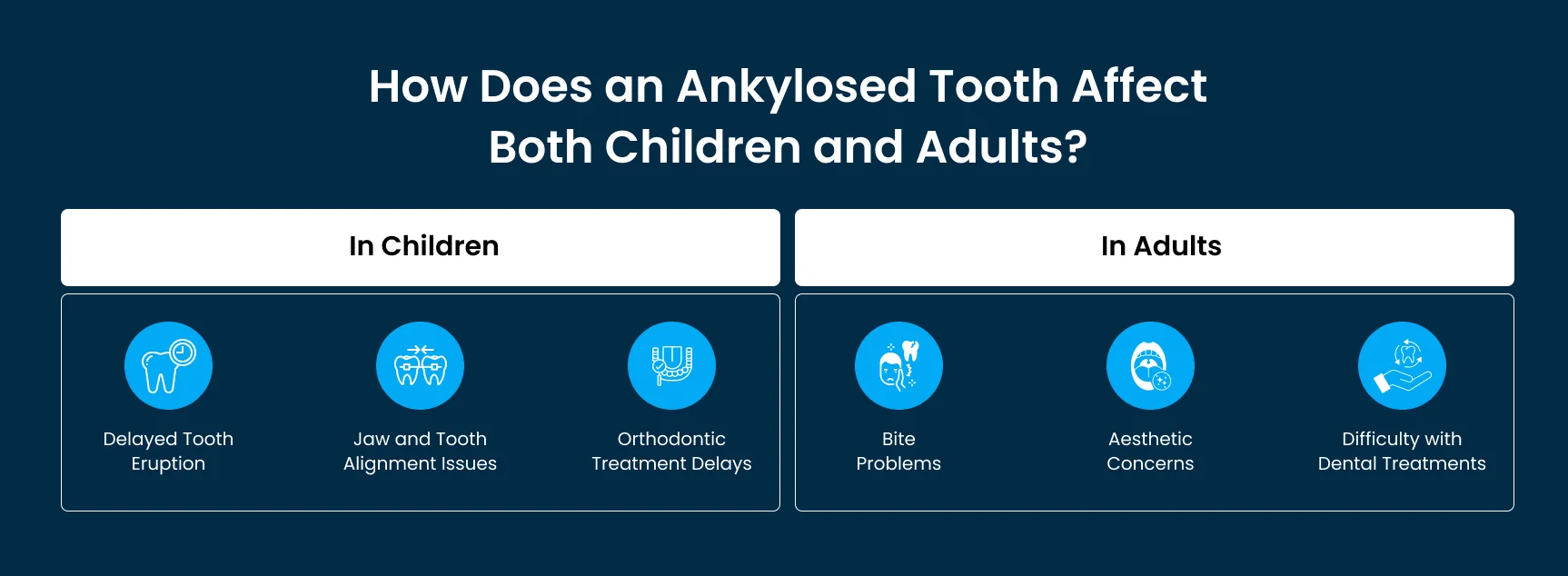
Children are still growing, so an ankylosed tooth can have a bigger impact on their overall dental development. For example:
In adults, the issue is slightly different since the jaw has already stopped growing. However, the condition still causes some unique challenges:
An ankylosed tooth happens when a tooth fuses directly to the jawbone, meaning it can’t move or grow like normal teeth. But what causes this to happen? Let’s break it down into a few key factors that can lead to ankylosis:
One of the most common causes is injury to the tooth or jaw. For example, if a child falls and injures their mouth, the tooth can be damaged. Over time, this injury can lead to the tooth fusing with the bone as it tries to heal. It's a bit like when a tree root grows into a crack in the sidewalk—the connection forms and becomes tough to separate.
A dental infection or untreated gum disease can also cause ankylosis. When the tissues around a tooth become inflamed or infected, it can damage the ligaments that normally keep the tooth mobile. Without these ligaments, the tooth may become stuck to the bone.
Some people are just more prone to ankylosed teeth due to their genetics. If someone in your family has had ankylosed teeth, you or your child might be at a higher risk. It’s similar to how certain other dental issues, like crooked teeth or jaw misalignment, can run in families.
Sometimes, ankylosis can develop as a result of orthodontic treatments or complications. If there’s a lot of pressure on a tooth due to braces or other appliances, it can occasionally cause the tooth to fuse to the bone. It’s not very common, but it’s something orthodontists keep an eye on.
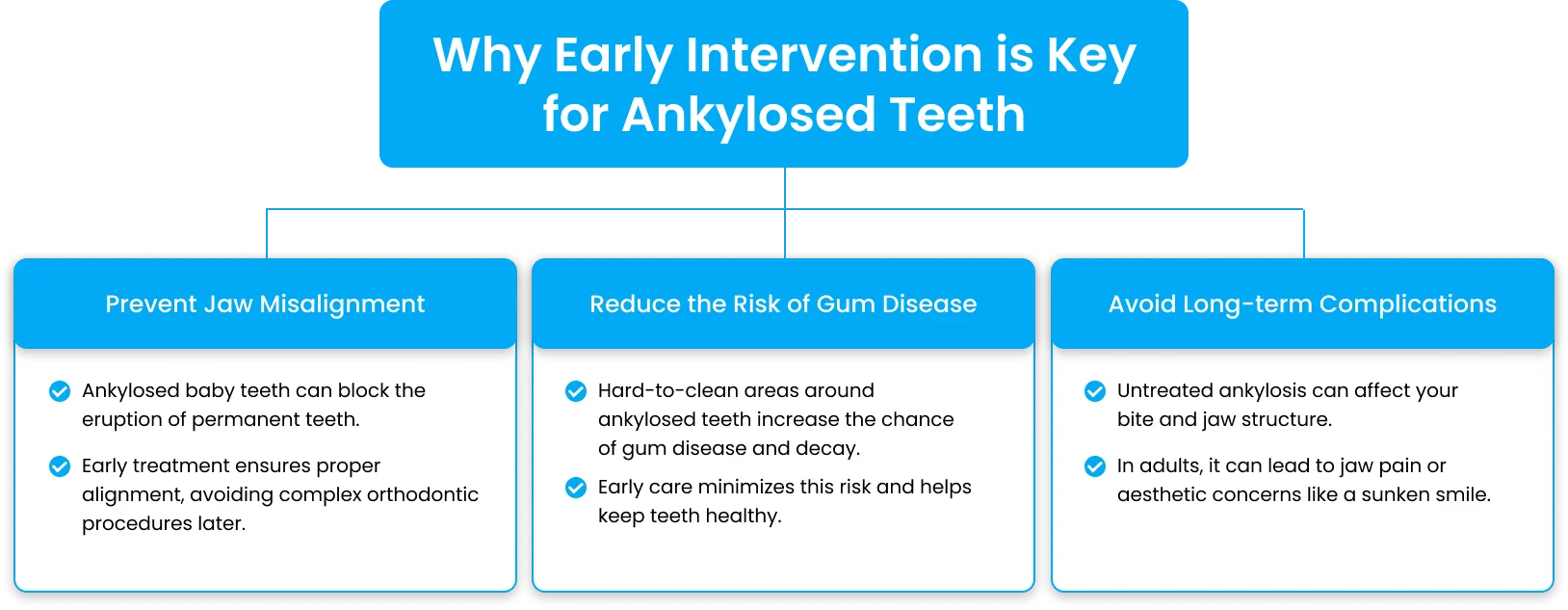
While some cases of ankylosis don’t cause immediate problems, it’s important to catch the condition early, especially in children. Here’s why:
Diagnosing an ankylosed tooth is important because, unlike a regular tooth, it doesn’t move or grow with the rest of the teeth. The diagnosis usually involves several steps that we perform during a routine checkup, but specific methods are used to confirm the condition.
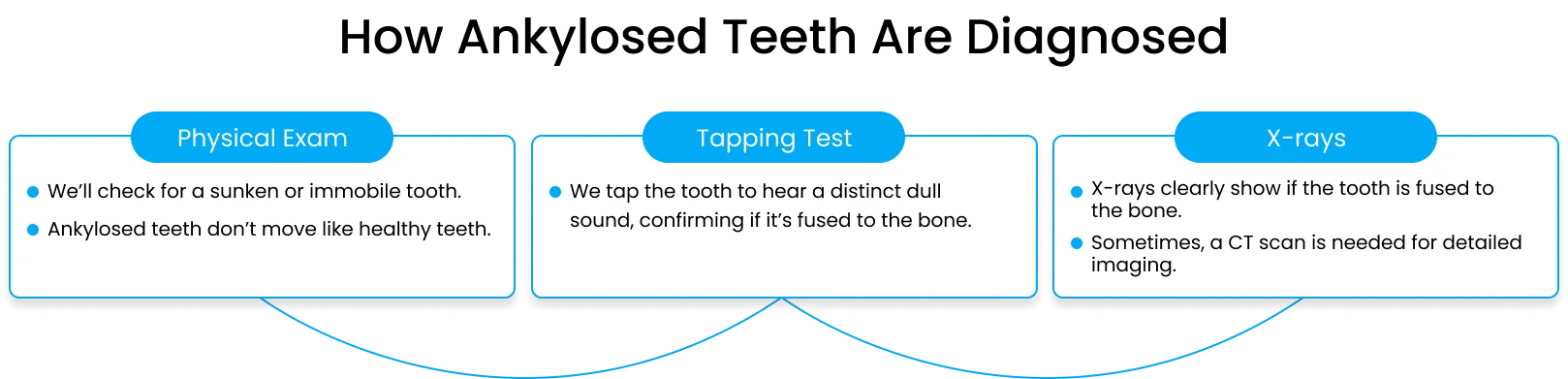
During a dental checkup, we look at the alignment and position of your teeth. If one tooth appears shorter or “sunken” compared to the others, it may raise suspicion. We might also check if the tooth seems firmly fixed in place, as ankylosed teeth lack the slight movement that healthy teeth typically have.
A tapping test is another method used by us. We gently tap the ankylosed tooth with an instrument to listen for a different sound compared to normal teeth. If the tooth is fused to the bone, it will produce a solid, dull sound, while a regular tooth will have a more cushioned sound due to the presence of the periodontal ligament, which normally separates the tooth from the bone.
An X-ray is one of the most effective ways to diagnose an ankylosed tooth. The X-ray will show whether the tooth is fused to the bone and if there is any missing space between the tooth and the surrounding bone. This method helps us to confirm the diagnosis and plan the next steps for treatment. Sometimes, a CT scan may be used for more detailed imaging, especially if the ankylosis is severe.
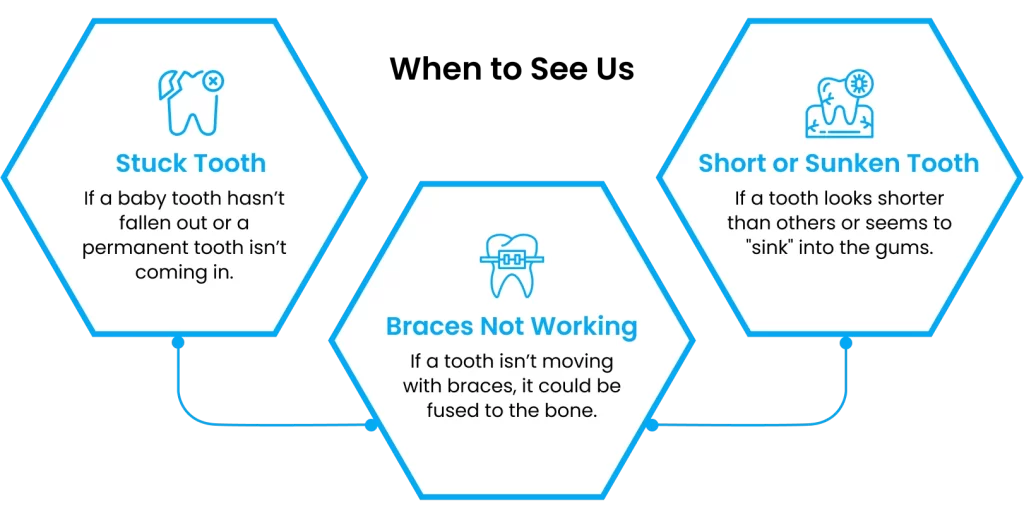
It can be difficult to know when a tooth is ankylosed, especially since there isn’t always immediate pain or discomfort. However, there are certain signs or concerns that should prompt you to visit the dentist:
Takeaway
If you notice any of these signs, visiting a dentist as soon as possible is essential. The earlier an ankylosed tooth is diagnosed, the better the chances of avoiding complications like jaw misalignment or delayed orthodontic treatment. We can confirm the diagnosis and discuss treatment options with a quick physical exam and an X-ray.
If you’re concerned about a tooth that seems out of place or isn’t moving as it should, don’t wait—get it checked out!
When it comes to treating an ankylosed tooth, the approach depends on several factors, such as the severity of the condition, the patient’s age, and whether the tooth is a baby or permanent tooth. Here’s a breakdown of the common treatment options, ranging from less invasive to more involved procedures.
In some cases, especially with ankylosed baby teeth, we may recommend a “wait-and-see” approach. If the tooth isn’t causing any significant problems, and the permanent tooth is likely to erupt normally, your dentist might simply monitor the situation.
When this works:
If the ankylosed tooth is causing more severe issues, such as blocking the eruption of permanent teeth, or if it’s a permanent tooth that is stuck, we might suggest surgical extraction. This is the most common treatment for moderate to severe cases, especially in children, as it prevents long-term problems like jaw misalignment.
How it works:
Concerns about pain and recovery:
Another less invasive option is luxation, where we attempt to break the fusion between the tooth and the bone without removing the tooth entirely. This allows the tooth to move or erupt naturally.
How it works:
This method works best for mild to moderate ankylosis, especially in children where the goal is to preserve the natural tooth and promote proper eruption or alignment.
In cases where ankylosis affects tooth alignment, orthodontic treatment is often required after the extraction or luxation of the ankylosed tooth. Braces or other orthodontic appliances are used to ensure the surrounding teeth move into the correct positions and that the jaw aligns properly.
Why orthodontics might be needed:
For more severe cases, particularly where the tooth needs to be repositioned rather than removed, a corticotomy may be performed. This involves cutting into the bone around the tooth to reposition it.
How it works:
This method is used when keeping the tooth is a priority, but orthodontic movement is impossible due to the fusion to the bone.
If a permanent ankylosed tooth is extracted and there’s a large gap left behind, dental implants or bone grafting may be needed. This is especially common in adults who want to restore both function and appearance.
How it works:
The treatment for an ankylosed tooth depends on the severity of the condition and the patient’s age. For mild cases, observation may be all that’s needed, but for more severe cases, surgical extraction or repositioning is often the best solution.
Addressing an ankylosed tooth early—especially in children—can prevent long-term issues like jaw misalignment, tooth crowding, and the need for more invasive treatments later on.
If you’re worried about the treatment process, your dentist will guide you through each step and ensure you’re comfortable, pain-free, and prepared for a smooth recovery.
After treating an ankylosed tooth—whether through extraction, luxation, or repositioning—there are a few key things to keep in mind for a smooth recovery. Proper post-treatment care is essential for healing, and in many cases, orthodontic treatment may still be needed to correct any alignment issues caused by the ankylosed tooth. Here’s what to expect after treatment:
What Happens After Ankylosed Tooth Treatment?
Diet:
Oral Hygiene:
Pain Management:
In many cases, especially if the ankylosed tooth caused crowding or misalignment, orthodontic treatment will continue after the tooth is extracted or repositioned.
Braces or Aligners:
Retainers
Monitoring Recovery:
Orthodontic Follow-Up:
4. Long-Term Outcomes
Most patients recover well from ankylosed tooth treatments with proper post-treatment care and regular follow-up visits. In children, early intervention often prevents more serious issues, such as jaw misalignment or tooth crowding. For adults, follow-up care ensures that the bite remains functional and aesthetically pleasing.
Taking care of your mouth after ankylosed tooth treatment is crucial for a smooth recovery. Following your dentist’s advice for post-treatment care, attending follow-up appointments, and continuing orthodontic treatments will help ensure the best long-term outcome.
If you have any concerns or notice something unusual during your recovery, don’t hesitate to reach out to your dentist for guidance!